We use some of the most advanced technology available to measure and image your eye with precision, allowing confidence when monitoring for change and allowing early diagnosis in many cases.
Imaging
Spectralis Optical Coherence Tomography (OCT)
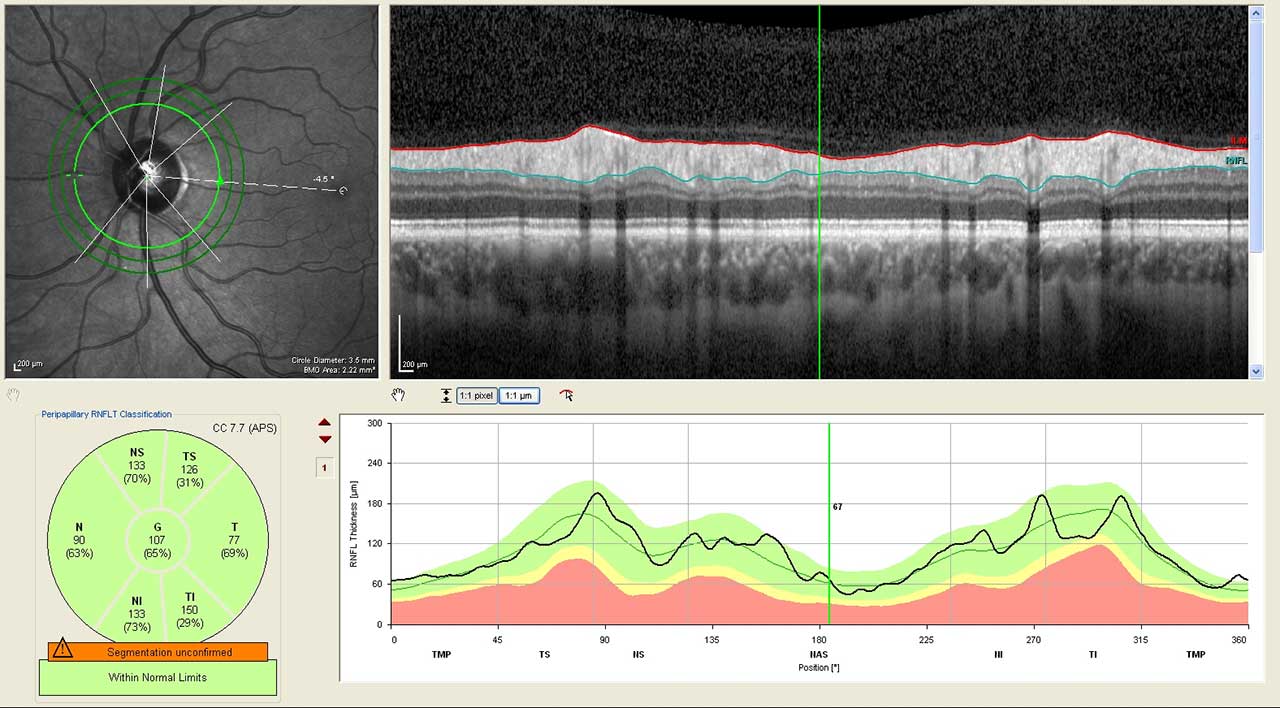
An OCT scanner uses reflection of light from the structures of the eye to build an extremely accurate and precise cross-sectional image. This device can image the cornea, the position of structures in the front of the eye, the retina and the optic nerve. In optic nerve problems such as glaucoma, the OCT allows us to measure the thickness or amount of nerve fibres entering the nerve from the retina.
The Spectralis is an outstanding device in a growing market of OCT machines, because it tracks the eye with unique precision so that repeated measurements are in exactly the same place. Optic nerve diseases such as glaucoma or retinal diseases can be diagnosed and monitored with much greater sensitivity and repeatability than a specialist with a traditional eye examination. With the most current software to analyse the scan results, we can now take advantage of the latest research into glaucoma diagnosis, other optic nerve conditions, retinal disorders, and more.
Heidelberg Retinal Topography
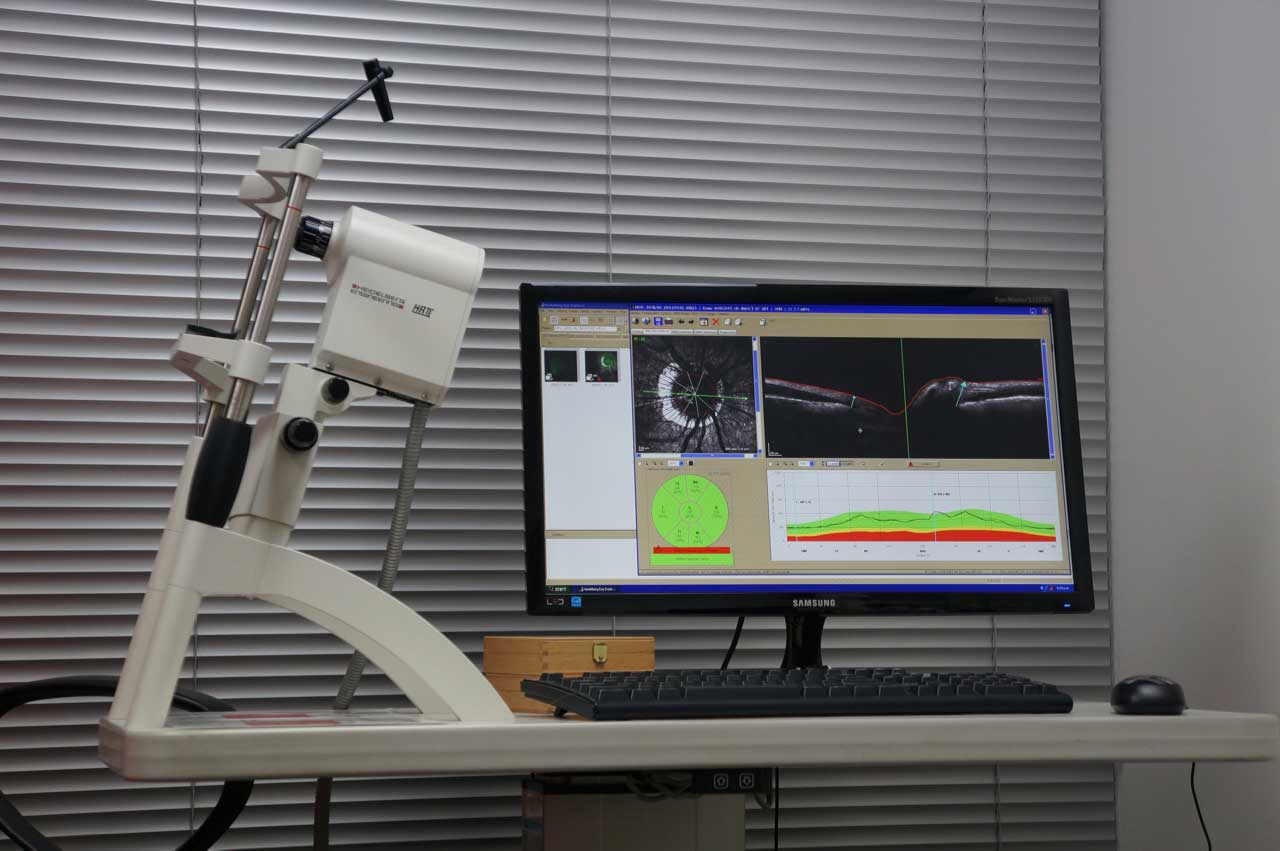
We have over 10 years experience using this machine that provides extremely sensitive information on changes in the shape of the optic nerve head, as occurs in glaucoma. By comparing the surface of the optic nerve head with excellent repeatability over time, very subtle changes can be detected which might indicate that preventive treatment is required before changes develop further to affect vision.
Anterior Segment Optical Coherence Tomography (AS OCT)
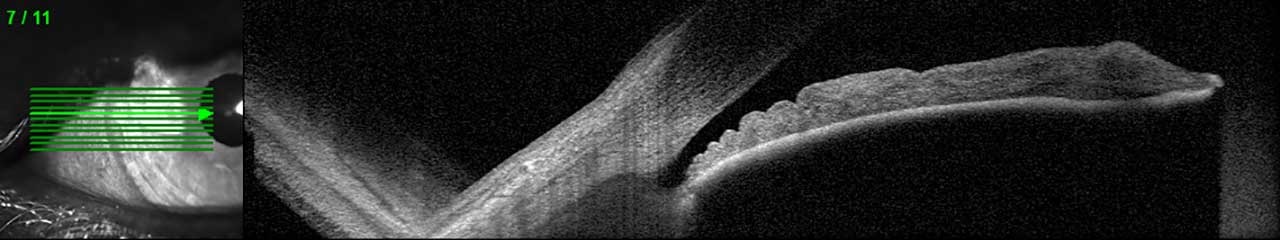
This OCT scanner examines the front of the eye, particularly the angle where the cornea (front window) and iris (coloured part of the eye) meet. This is the area through which fluid drains out of the eye. These OCT images show us how close the iris is to blocking the drainage of fluid out of the eye, and help guide us about whether laser treatment may be needed.
Retinal photography
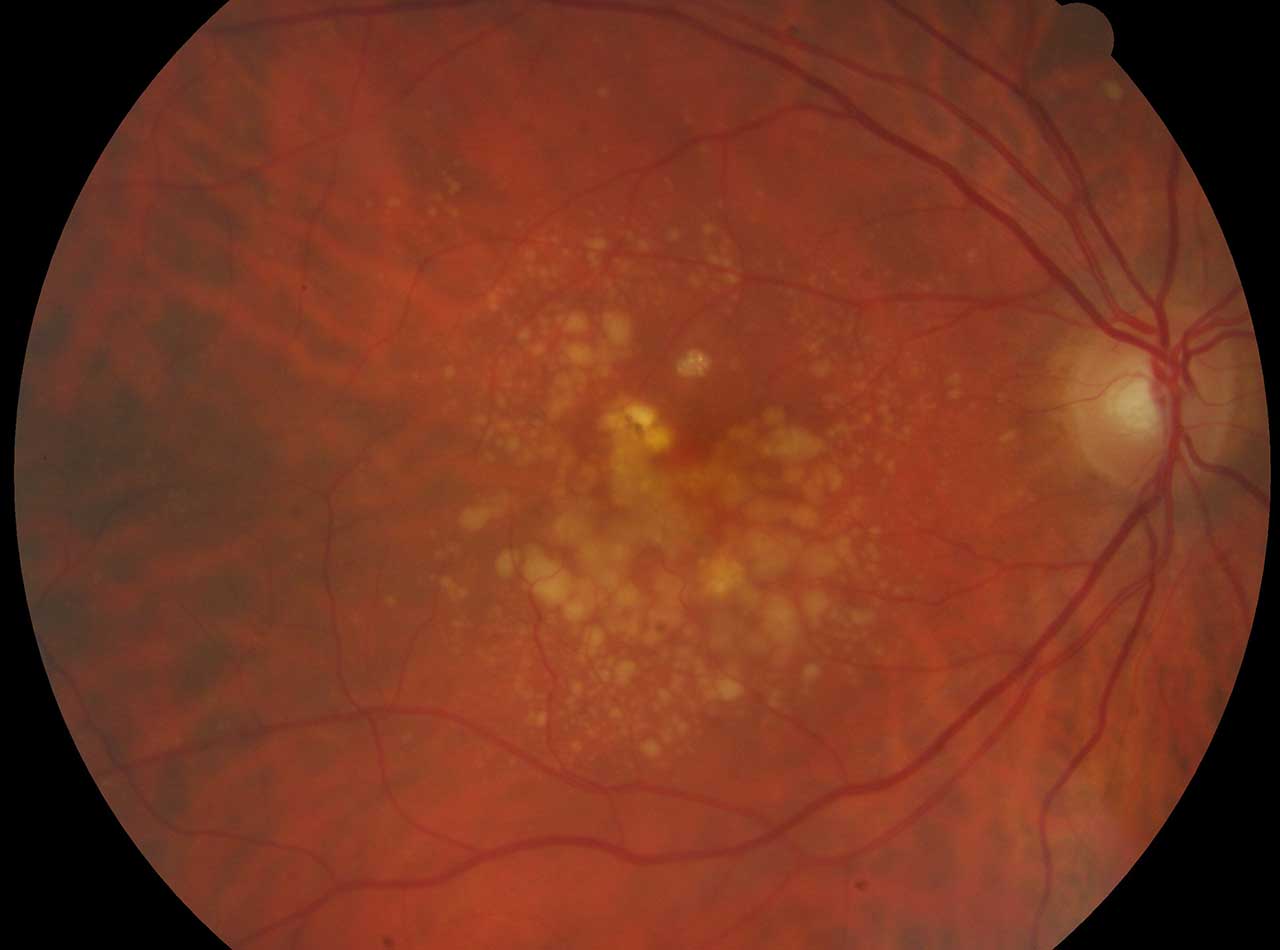
Photos of the retina are useful for keeping a record, as well as for showing and explaining what is happening. These pictures can be especially useful in conditions where a slow change might be important, such as monitoring a naevus of the choroid (similar to having a mole map for freckles on the skin).
Visual field testing
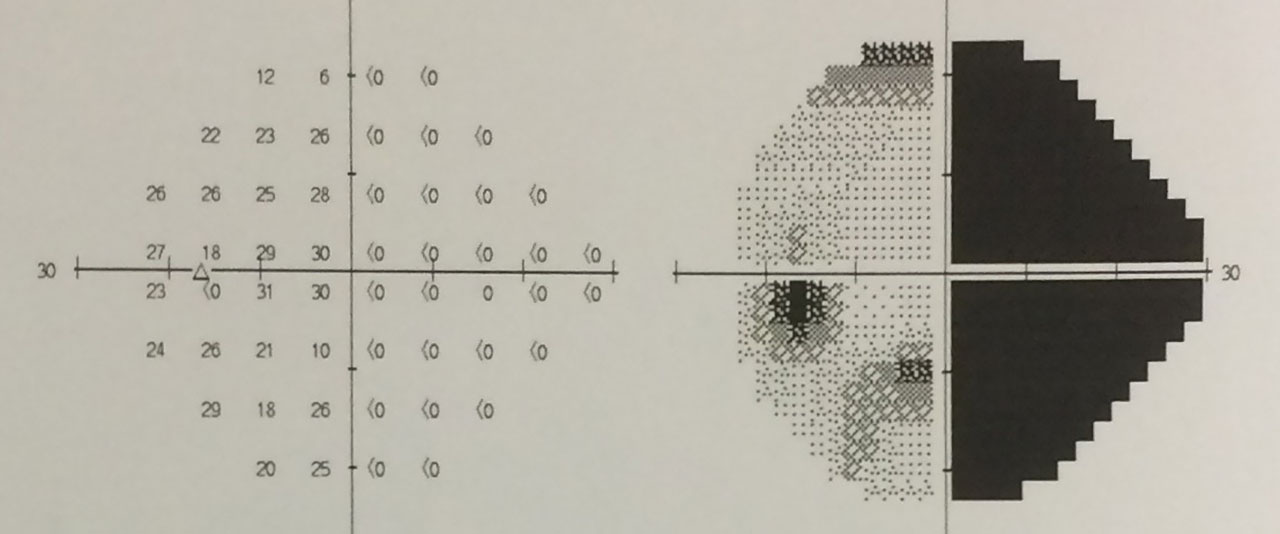 A visual field test gives us detailed information about the sensitivity of both the central and peripheral vision. They are an important measure of the function of the eye and entire visual pathway to the brain, so visual field tests can reveal a diagnosis when the eye looks normal. In glaucoma the visual field is affected long before the central vision and patients are usually unaware of this field loss until it is advanced. The test experience is similar to a very basic and boring video game. Our machine presents shimmering lights in your central and peripheral vision and you are asked to press a button when you see one.
A visual field test gives us detailed information about the sensitivity of both the central and peripheral vision. They are an important measure of the function of the eye and entire visual pathway to the brain, so visual field tests can reveal a diagnosis when the eye looks normal. In glaucoma the visual field is affected long before the central vision and patients are usually unaware of this field loss until it is advanced. The test experience is similar to a very basic and boring video game. Our machine presents shimmering lights in your central and peripheral vision and you are asked to press a button when you see one.
Ocular biomechanics
Our clinic has devices to measure the intraocular pressure in different ways, and to measure the thickness of the cornea, and together these give information about how easily the eye is stretched by pressure. Some clinical studies indicate that these factors can predict the likelihood of developing glaucoma. The emerging understanding is that the way in which an eye stretches in response to pressure partly determines how much that pressure damages the optic nerve in glaucoma.
Specular microscope
This device creates a microscopic image of the cells lining the inside of the cornea. These cells are of particular importance to keep the cornea clear. This device allows more accurate diagnosis of some corneal problems, and we are using the images in research to ensure that laser and surgical procedures are safe in the long term.
Ultrasound biomicroscope

Our clinic has an ultrasound machine for measuring and imaging the eye. The ultrasound biomicroscope is a specialized device for imaging very small structures in the front of the eye, and in certain situations it can be crucial for diagnosis. The ultrasound can also be used to measure the eye before cataract surgery, and can diagnose problems in the back of the eye that can’t be seen or measured by examination.
Biometry for cataract surgery
Cataract surgery is the most common eye operation, and today we all expect very high standards of visual outcome. Before surgery, the eye must be measured to choose an intraocular lens that is predicted to give the desired focus after surgery. The latest devices for measuring the eye, such as the IOL Master 700 at Capital Eye Specialists, use a laser to precisely measure the length of the eye, and provide several accurate measurements of the front of the eye as well.
Laser treatments
Selective Laser Trabeculoplasty (SLT)
Most commonly in glaucoma or ocular hypertension, the drainage structure of the eye (the trabecular meshwork) appears normal but is not functioning at full capacity, so the eye pressure is higher than normal. The SLT laser applies extremely short bursts of laser energy to improve the function of these trabecular meshwork cells, without leaving any visible scars or permanent injury. It could be described as stimulating these drainage cells to work harder.
In general SLT has similar effectiveness to eye drops. Because there are no permanent scars, it is considered safe and effective to repeat treatment when needed in the future. In some cases SLT is the only treatment required and may allow patients to stop their glaucoma drops or in other cases it may reduce the number of drops or lower the pressure to a safe level while drops continue. In every case regular monitoring is still required.
YAG laser peripheral iridotomy
Some people have eyes where the iris (coloured part) and cornea (clear front window) are in close proximity. When the iris is so close to the cornea that it can block outflow of fluid from the eye, we call this angle closure, and this can sometimes lead to high eye pressure or glaucoma. The first step in treating angle closure is to perform an iridotomy.
The YAG laser has a “flicking” action inside the eye, and creates a tiny hole in the edge of the iris, invisible from the outside and this should not affect vision at all. The hole allows the iris to rest back away from the cornea, creating more space around the drainage structure of the eye. Usually after the treatment anti-inflammatory drops are used for a week.
Diode laser peripheral iridoplasty
In some situations where angle closure persists after an iridotomy, we may recommend this procedure. It involves placing about 30 small burns on the edge of the iris with a different type of laser. These burns contract and thin the iris (they do not create a hole), and the effect is to pull the iris away from the cornea and drain of the eye.
YAG laser capsulotomy
After cataract surgery the new plastic intraocular lens sits within the clear cellophane-like capsule bag from which the cataract has been removed. Months to years later, some patients develop thickening and cloudiness of this capsule, which may blur the vision again. The YAG laser can be used to cut a hole in the cloudy capsule without disturbing the plastic lens or the front of the eye, so that light is once again able to pass clearly to the retina.
Diode laser transcleral ciliary ablation (cyclodiode)
In some types of glaucoma with high pressures despite glaucoma surgery and medications, or when surgery is inappropriate for some reason, a cyclodiode treatment can be performed to reduce the production of fluid in the eye. The laser shines through the white sclera, just outside the clear cornea, and is absorbed by the pigmented structures inside that produce fluid (the ciliary body). A series of burns reduces the production of fluid in the eye. Inflammation is usual, so anti-inflammatory drops are required afterward. This treatment is usually given after other treatments have been tried.
